A New Dawn for Spinal Cord Injury Repair: The Neuroregeneration Revolution
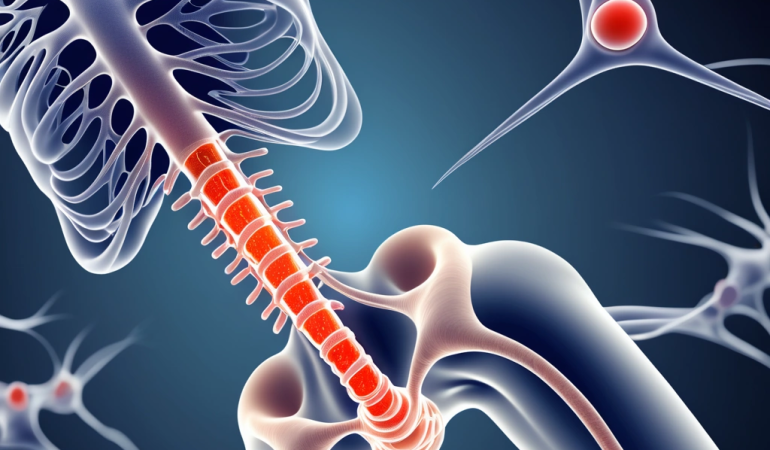
The quest to mend the severed connections of the spinal cord, once relegated to the realm of science fiction, is rapidly gaining ground in reality. Spinal cord injury (SCI), a devastating condition affecting millions worldwide, has long been considered an irreversible neurological catastrophe. However, a surge of innovation in neuroregeneration technologies offers unprecedented hope. From stem cell therapies that aim to replace damaged cells to gene therapies designed to reactivate dormant regenerative pathways and biomaterial scaffolds that provide a framework for regrowth, the landscape of SCI repair is undergoing a seismic shift.
This article delves into these cutting-edge approaches, analyzing their mechanisms, clinical trial outcomes, and the ethical considerations that accompany this transformative field. This new dawn in neurological enhancement is fueled by breakthroughs in regenerative medicine, offering the potential to restore lost function and improve the quality of life for individuals affected by spinal cord injury. “We are witnessing an unprecedented convergence of scientific disciplines, from molecular biology to materials science, all focused on unlocking the spinal cord’s regenerative potential,” notes Dr.
Emily Carter, a leading neuroscientist at the forefront of SCI repair research. The convergence of these fields is accelerating the development of novel therapies and pushing the boundaries of what was once considered impossible. Among the most promising avenues is personalized medicine, tailoring treatments to the unique characteristics of each patient’s injury. Advanced neuroimaging techniques, combined with sophisticated data analysis, are enabling clinicians to gain a deeper understanding of the individual factors that influence recovery.
This personalized approach allows for the selection of the most appropriate therapies and the optimization of treatment strategies, maximizing the potential for neuroregeneration and functional improvement. The integration of artificial intelligence and machine learning is further enhancing our ability to predict treatment outcomes and personalize interventions. Despite the significant progress, challenges remain in translating preclinical successes into robust clinical outcomes. The complexity of the spinal cord microenvironment and the limited capacity for spontaneous regeneration pose significant hurdles. However, ongoing clinical trials are providing valuable insights into the safety and efficacy of various neuroregeneration strategies. These trials are not only evaluating the potential of stem cell therapy, gene therapy, and biomaterial scaffolds but also exploring novel combinations of these approaches to achieve synergistic effects. The future of SCI repair lies in a multi-faceted approach that combines cutting-edge technologies with a deep understanding of the individual patient’s needs.
The Arsenal of Neuroregeneration: Stem Cells, Genes, and Scaffolds
Several promising avenues are being explored to promote neuroregeneration after SCI. Stem cell therapy, perhaps the most widely recognized, involves transplanting cells with the potential to differentiate into various neural cell types. These cells can replace damaged neurons, oligodendrocytes (which produce myelin, the insulating sheath around nerve fibers), and astrocytes. Clinical trials have focused on various stem cell sources, including embryonic stem cells, induced pluripotent stem cells (iPSCs), and mesenchymal stem cells (MSCs). While some studies have shown modest improvements in motor function and sensory perception, significant challenges remain, including cell survival, integration into the host tissue, and the risk of tumor formation.
Recently, anecdotal discussions surrounding celebrities undergoing stem cell therapy have surfaced, highlighting the growing public interest. However, the scientific community emphasizes that rigorous, controlled clinical trials are essential to validate the efficacy and safety of these treatments for SCI repair. These trials must address critical factors such as optimal cell dosage, delivery methods, and long-term monitoring to ensure genuine neurological enhancement. Gene therapy offers another compelling strategy in the arsenal of neuroregeneration. By delivering genes that encode for growth factors, neurotrophic factors, or proteins that inhibit scar formation, researchers aim to create a more permissive environment for axonal regeneration.
For example, introducing genes that promote the expression of chondroitinase ABC, an enzyme that breaks down chondroitin sulfate proteoglycans (CSPGs) – major components of the glial scar – has shown promise in preclinical studies. Clinical trials are now underway to evaluate the safety and efficacy of gene therapy approaches in humans with SCI. Companies like Novartis and Genentech are investing heavily in gene therapy research for neurological disorders, signaling a growing confidence in its potential for SCI repair.
The key lies in developing targeted delivery systems that can efficiently transduce cells within the spinal cord while minimizing off-target effects. Biomaterial scaffolds provide a three-dimensional matrix that can support cell growth, guide axonal extension, and deliver therapeutic agents. These scaffolds can be made from a variety of materials, including natural polymers like collagen and laminin, as well as synthetic polymers like poly(lactic-co-glycolic acid) (PLGA). The ideal scaffold should be biocompatible, biodegradable, and possess mechanical properties that mimic the native spinal cord tissue.
Researchers are also incorporating growth factors, cell adhesion molecules, and other bioactive cues into scaffolds to further enhance their regenerative potential. Innovative designs include incorporating microchannels to guide axonal growth and creating porous structures that allow for vascularization, crucial for cell survival and integration. These biomaterial scaffolds represent a critical component of regenerative medicine strategies, offering a structural and biochemical bridge across the injury site. Beyond these core strategies, the convergence of multiple approaches is gaining traction.
Combining stem cell therapy with gene therapy, for instance, could create a synergistic effect, where stem cells deliver therapeutic genes directly to the injury site. Similarly, integrating biomaterial scaffolds with drug delivery systems allows for sustained release of neurotrophic factors, promoting long-term neuroregeneration. This multi-faceted approach reflects a growing understanding of the complex interplay of factors that contribute to SCI and the need for personalized medicine strategies that address the unique characteristics of each injury.
The future of SCI repair lies not in a single magic bullet, but in a carefully orchestrated combination of technologies tailored to the individual patient. Furthermore, the field is witnessing a surge in research focused on modulating the immune response following SCI. The inflammatory cascade that ensues after injury can exacerbate neuronal damage and hinder neuroregeneration. Strategies aimed at suppressing detrimental inflammation while promoting a pro-regenerative immune environment are showing promise in preclinical studies. These include the use of immunomodulatory drugs, engineered immune cells, and biomaterials that can modulate immune cell behavior. Integrating these immunomodulatory approaches with other neuroregeneration strategies could significantly enhance SCI repair outcomes. This holistic approach, addressing both the neurological and immunological aspects of SCI, represents a crucial step forward in the quest for effective treatments.
Clinical Trials: Hope, Hype, and Hard Realities
The translation of neuroregeneration technologies from the laboratory to the clinic has been met with both excitement and cautious optimism. While preclinical studies in animal models have demonstrated remarkable regenerative capabilities, clinical trials in humans have yielded more modest results. A major hurdle is the inherent complexity of SCI, which involves not only neuronal damage but also inflammation, scar formation, and vascular disruption. Moreover, the timing of intervention, the severity of injury, and the age of the patient can all influence treatment outcomes.
This complexity underscores the need for personalized medicine approaches in SCI repair, tailoring interventions to individual patient profiles. Analysis of clinical trial data reveals a mixed bag of results. Some studies have reported statistically significant improvements in motor function, sensory perception, and bowel/bladder control in patients treated with stem cell therapy. However, these improvements are often small and may not translate into meaningful functional gains. Gene therapy trials, while demonstrating safety and tolerability, are still striving to provide definitive efficacy data.
Biomaterial scaffold studies are in their early stages, but initial results suggest that these devices can promote tissue integration and axonal sprouting, offering a structural bridge for neuroregeneration. It is important to emphasize that many clinical trials are still ongoing, and larger, randomized controlled studies are needed to determine the true potential of these therapies. The variability in patient responses highlights the necessity of refined patient selection criteria and outcome measures in future clinical trials.
Recent research highlights the role of astrocytes in neural repair, with a study titled ‘Astrocytes gain neural stem cell properties after brain injury’ suggesting that astrocyte plasticity, correlated with Galectin 3 protein upregulation, may contribute significantly to biomarker discovery. This could lead to improved diagnostic and therapeutic strategies for SCI. Furthermore, advancements in understanding the molecular mechanisms underlying astrocyte reactivity could pave the way for novel therapeutic targets aimed at modulating scar formation and promoting a more permissive environment for axonal regeneration.
This focus on glial cells, alongside neuronal repair strategies, represents a crucial step towards comprehensive SCI repair. Beyond traditional clinical trials, innovative trial designs are emerging to accelerate the evaluation of neuroregeneration strategies. Adaptive clinical trials, for example, allow for modifications to the treatment protocol based on interim data, potentially shortening the time required to identify effective therapies. Real-world evidence, gathered from patient registries and electronic health records, can also provide valuable insights into the long-term outcomes of different interventions. These advancements in clinical trial methodology, coupled with a deeper understanding of the pathophysiology of spinal cord injury, are crucial for translating the promise of neuroregeneration into tangible benefits for patients.
The Future is Personalized: Convergence, Nanotechnology, and Ethical Frontiers
The future of neuroregeneration for SCI lies in personalized medicine approaches that tailor treatments to the individual patient’s specific injury profile. This includes considering factors such as the level and severity of injury, the time since injury, the patient’s age and overall health, and their genetic background. Advances in neuroimaging, biomarker discovery, and computational modeling will enable clinicians to better predict treatment outcomes and optimize therapeutic strategies. For instance, sophisticated MRI techniques can now visualize the extent of spared neural tissue at the injury site, offering crucial insights for tailoring stem cell therapy or gene therapy interventions.
Identifying specific biomarkers in cerebrospinal fluid or blood can also provide real-time feedback on the efficacy of regenerative medicine approaches, allowing for timely adjustments to treatment protocols. These personalized approaches represent a significant departure from the ‘one-size-fits-all’ model, promising more effective and targeted SCI repair. Furthermore, the convergence of multiple neuroregeneration technologies holds great promise. For example, combining stem cell therapy with gene therapy or biomaterial scaffolds may create a synergistic effect that enhances regeneration.
Consider the potential of using genetically modified stem cells, delivered via a biodegradable scaffold, to secrete growth factors directly at the injury site. This trifecta approach could simultaneously replace damaged cells, stimulate axonal regrowth, and provide structural support for new neural connections. Nanotechnology also has the potential to revolutionize SCI repair by enabling targeted drug delivery, precise tissue engineering, and real-time monitoring of neural activity. Imagine nanoparticles carrying regenerative drugs directly across the blood-spinal cord barrier, or nanosensors tracking the electrophysiological activity of newly formed synapses.
These innovations could dramatically improve the precision and efficacy of SCI treatments. Recent breakthroughs in understanding the molecular mechanisms underlying axonal regeneration are also paving the way for novel therapeutic targets. For example, research has identified several key signaling pathways that inhibit axonal growth after SCI, such as the Rho/ROCK pathway. Developing drugs that specifically target these inhibitory pathways, in combination with other regenerative strategies, could unlock the inherent capacity of neurons to regrow and reconnect.
Another promising area of investigation is the use of electrical stimulation to promote axonal sprouting and plasticity. Studies have shown that applying specific patterns of electrical stimulation to the spinal cord can enhance the effects of rehabilitation therapy and improve motor function in individuals with SCI. These advances highlight the importance of a multi-faceted approach to neuroregeneration, combining molecular, cellular, and technological interventions to maximize recovery. However, the development of neuroregeneration technologies also raises important ethical considerations.
The potential for neurological enhancement, rather than just restoration, raises questions about fairness, access, and the definition of disability. It is crucial to have open and transparent discussions about the ethical implications of these technologies to ensure that they are used responsibly and equitably. The role of government healthcare policies, such as those of PhilHealth for Overseas Filipino Workers (OFWs), in providing access to these potentially life-changing but often expensive treatments also needs careful consideration. The challenge lies in ensuring that these innovative therapies are available to all who could benefit, regardless of their socioeconomic status, while also safeguarding against unintended consequences and upholding the principles of autonomy and justice.
Toward a Future of Recovery: Embracing the Promise of Neuroregeneration
The journey to conquer spinal cord injury is far from over, but the progress made in neuroregeneration technologies offers a beacon of hope for individuals living with this debilitating condition. While challenges remain in translating preclinical success into robust clinical outcomes, the ongoing research and development efforts are paving the way for a future where SCI is no longer considered an irreversible tragedy. By embracing personalized medicine approaches, fostering collaboration between researchers and clinicians, and addressing the ethical considerations that arise with these powerful technologies, we can unlock the full potential of neuroregeneration and transform the lives of millions affected by SCI.
The convergence of stem cell therapy, gene therapy, and biomaterial scaffolds represents a particularly exciting frontier in SCI repair. For example, researchers are exploring the use of injectable scaffolds that not only provide structural support for regenerating axons but also deliver growth factors and other therapeutic agents directly to the injury site. This multi-pronged approach aims to overcome the complex challenges of SCI, including inflammation, scar tissue formation, and the limited intrinsic regenerative capacity of the central nervous system.
One of the most promising avenues in personalized medicine for spinal cord injury involves leveraging advanced neuroimaging techniques to precisely characterize the extent and nature of the injury. This allows clinicians to tailor treatment strategies to the individual patient’s specific needs, maximizing the potential for neurological enhancement. For instance, a patient with a relatively recent and incomplete SCI might benefit most from aggressive rehabilitation combined with targeted gene therapy to promote axonal regrowth, while a patient with a chronic and complete SCI might be a better candidate for stem cell transplantation to replace lost neurons and restore some level of function.
Furthermore, ongoing clinical trials are crucial for validating the safety and efficacy of these innovative therapies and for identifying biomarkers that can predict treatment response. The careful design and execution of these trials are essential for advancing the field of regenerative medicine and ensuring that new treatments are both effective and accessible to those who need them most. Looking ahead, the integration of nanotechnology into neuroregeneration strategies holds immense promise. Nanoparticles can be engineered to deliver drugs, genes, or proteins directly to specific cells within the injured spinal cord, minimizing off-target effects and maximizing therapeutic impact.
Moreover, nanoscale scaffolds can be designed to mimic the natural extracellular matrix, providing an optimal environment for axonal regeneration and neuronal survival. However, as with any emerging technology, it is crucial to carefully consider the ethical implications of neuroregeneration. Questions surrounding access to these potentially life-changing therapies, the potential for unintended consequences, and the definition of what constitutes a ‘successful’ outcome must be addressed proactively to ensure that these technologies are used responsibly and equitably. The future of SCI repair lies not only in scientific breakthroughs but also in a commitment to ethical innovation and patient-centered care.